Trainer´s considerations during the workout
We can consider that moderate-intensity exercise will reduce glucose serum levels while high-intensity exercise will increase serum glucose levels.
Despite this consideration, we have to pay attention to non-trained patients. In these people, an excess of hepatic glucose production may occur caused by a non-accurate exercise response. It can happen during moderate-intensity exercise, so trainers should monitoring all possible symptoms of hyperglycemia and measure patient´s glucose levels during the first phases of a training program.
We have to pay special attention when exercise intensity reaches the lactate threshold. In this point, dramatic production of catecholamines, ketones and free fatty acids will reduce or impair muscle glucose metabolism. All these factors will produce an increase in blood glucose levels. The action of counterregulatory hormones, but most T1DM patients may need a bolus administration to help them to regulate these values.
A similar situation may occur in performance athletes, mostly during intermittent sports. The pre-competition stress (catecholamines) and the resting periods between high-intensity exercise bouts may cause longer hyperglycemia than during training days. Is very important to analyze the glucose curves during training days and compare them with competition days to create an insulin administration system to prevent any complication. This can be especially important for youth athletes.
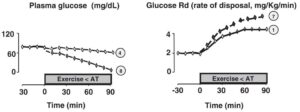
Glucose homeostasis during moderate exercise in T1DM
The trainer should know the behaviour of glucose metabolism during moderate and intense exercise un T1DM patients.
Depending on the type of exercise programmed, different actions must be developed before during and after the workout/competition.
The first step is to compare the insulin-glucose metabolism of a T1DM patient to a healthy subject.



![]()
During moderate long term exercise, insulin regulation is “inadequate” due to the administration of external insulin and the insulin storage in injected tissue. Insulin will be constant or increased during exercise. This fact promotes a glucose decrease which can be exacerbated due to the bad endogenous glucose production.
Trainers should analyze the glucose curves of the athlete and teach him/her (directed by a physician) how to adminístrate glucose before and during exercise to avoid the hypoglycemic.
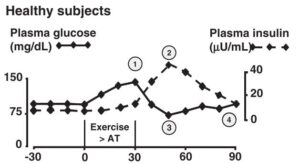
Glucose homeostasis during intense exercise in T1DM patients
When we prescribe high intensity exercise, is very important to avoid the risk of hyperglicemic reaction.
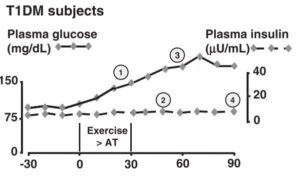
Let´s analyze the insulin glucose behaviour of T1DM patient compare to a control subject.


![]()
Healthy subjets are able to adjust both insuline and glucose during exercise. This regulation results in a continous and controled change between both parameters. When the endogenous glucose production is too high, the metabolism reacts, rising insulin plasma levels and which promote a natural balance.
In T1DM patients this balance is not posible and the endogenous glucose production can not be stoped by the endogenous production of insulin. The process results in a hyperglicemic state.
Thus, is necesary the administration of fast insulin to regulate the insulin-glucose metabolism in T1DM patients who practice intense exercise. The momento and dose of this insulin should be prescribed and controled by experts.
Trainers should keep in contact with health specialist and teach athletes the physician instructions. Trainers should manage and control athlete’s behaviours to warranty their safety and performance.
Mix moderate and intense exercise. An effective strategie to follow.
The opposite effects of moderate and intense exercise can be combined to regulate the insulin-glucose metabolism during exercise in T1DM patients.
So much so, that the correct balance of prolonged, moderate exercise, and brief, intense exercise could induce opposing hypo- and hyperglycemic stimuli that would largely cancel each other out, and result in optimal glycemic control.
Exercise volumen, intensity and the lenth of each intensity period should be prescribed in an individual way. First evaluation and progressions should be directed by a health specialist.
Contraindications during exercise.
We have to know and teach to our athletes the main symptoms that may occur during the exercise sesion. If any of these symptoms appear exercise should be stoped and the patient should consult automatically a physician.
This symptoms are specially important for patient with cardiovascular risk diagnostic.
Typical and Atypical or Variant Symptoms of CVD in Persons with Diabetes Mellitus
1 Pain or discomfort in the chest, neck, jaw, arms, or other areas that may be due to myocardial ischemia (lack of adequate circulation)
2 Difficulty completing usual tasks
3 Dizziness with activity
4 Dyspnoea with minimal exertion
5 Orthopnea (breathing discomfort when not in an upright position) or paroxysmal nocturnal dyspnea (interrupted breathing at night 6 Ankle edema (swelling)
7 Palpitations (abnormal rapid beating of the heart) or tachycardia (rapid heartbeat)
8 Intermittent claudication (cramping pain and weakness in legs, especially calves, during walking due to inadequate blood supply to muscles)
9 Easy fatigability
10 Lack of energy 11 Neck or jaw discomfort 12 Shoulder pain with a history similar to bursitis and related to activity
Modified from (ACSM guidelines for exercise testing and prescription; Hughes & White, 2005)
BIBLIOGRAPHY
- Galassetti P, Riddell MC. Exercise and type 1 diabetes (T1DM). Compr Physiol. 2013;3(3):1309–36.


